
Poop & Weight Loss/Gain: How Your Bowel Health Impacts Your Scale
Your scale isn’t measuring fat — it’s measuring what your gut hasn’t let go of. Hidden stool retention, slow motility, and gut bacteria can quietly

Home » The Impact of Over-the-Counter Medicine on Gut Health: What You Need to Know
Imagine a day where your head pounds with pain, your stomach churns with discomfort, or a relentless cold leaves you weak and weary. You reach into your medicine cabinet, pull out an over-the-counter (OTC) remedy, and within minutes, relief washes over you. Sounds familiar, right? These little miracle pills, syrups, and tablets are the unsung heroes of our daily lives, offering quick fixes for a myriad of ailments. But what if I told you that while they’re solving one problem, they might be quietly creating another? Specifically, one that lurks deep in your gut.
Welcome to the intricate world of gut health, where billions of bacteria dance in a delicate balance, maintaining your health in ways you might not even realize. Yet, this balance is fragile, easily disrupted by factors we often overlook—like the OTC medicines we take for granted. In this post, we’ll dive into how these everyday medications, while convenient, might be doing more harm than good to your gut. By the end, you’ll not only be more informed about what you’re putting into your body but also empowered to make choices that protect your gut health and overall well-being.
What are OTC Medications?
Over-the-counter medications are the unsung workhorses of modern medicine. Unlike prescription drugs, which require a doctor’s blessing, OTC medications are available at your local pharmacy, grocery store, or even gas station, ready to leap into action whenever a headache, stomach ache, or cold threatens to derail your day. They are the first line of defense for millions of people around the world, providing fast and accessible relief from a host of minor ailments.
But what exactly qualifies as an OTC medication? Simply put, these are drugs that have been deemed safe and effective by regulatory agencies like the FDA when used according to the label instructions. They’re formulated to address common health issues that don’t necessarily require a doctor’s intervention. Pain relievers like ibuprofen or acetaminophen, antacids, cough syrups, allergy medications, and even certain sleep aids all fall into this category.
Yet, while the convenience of OTC medications is undeniable, their ease of access can sometimes lead to misuse or overuse. We often pop a pill without a second thought, trusting that because it’s available without a prescription, it must be harmless. However, as we’ll explore, the reality is more complex, especially when it comes to how these medications interact with our gut health.
Common OTC Medications and Their Ingredients
Let’s take a closer look at some of the most popular OTC medications and what they’re made of. This will help us understand how they work and, more importantly, how they might affect our gut.
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs)
Acetaminophen
Antacids and Acid Suppressants
Laxatives
Cold and Allergy Medications
Each of these medications serves a specific purpose and can be incredibly effective when used correctly. However, their effects don’t stop at the symptom they’re treating. The ingredients in these medications can have broader impacts, particularly on the gut—a part of the body that, as we’ll see, plays a crucial role in our overall health.
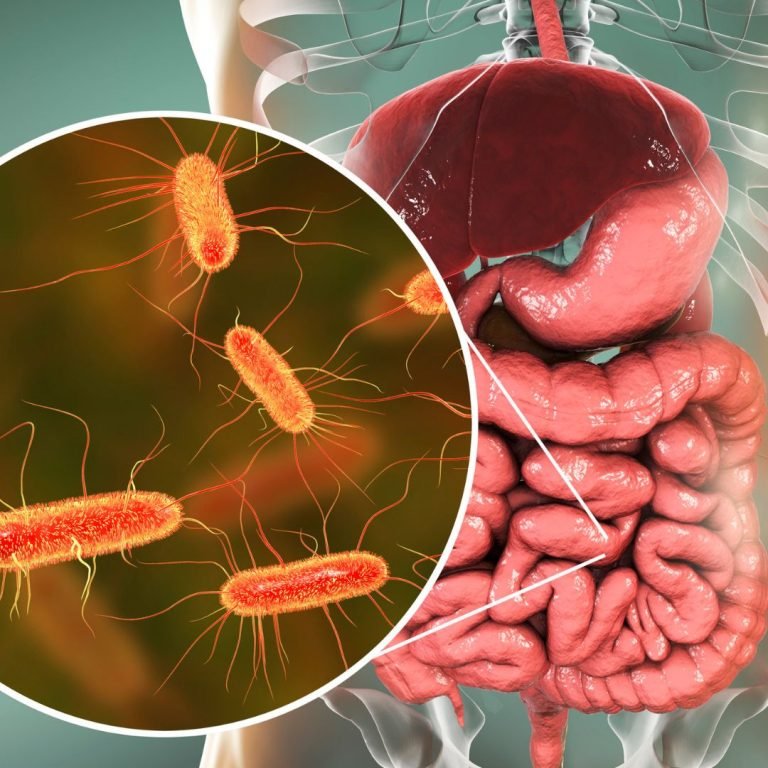
What is the Gut Microbiome?
If you’ve ever thought of your gut as just a simple digestive tract, it’s time to think again. Inside your gut lies one of the most complex and vital ecosystems in your body: the gut microbiome. This community of trillions of microorganisms—including bacteria, viruses, fungi, and other microbes—lives primarily in your intestines, influencing everything from digestion to immunity, and even your mood.
The gut microbiome is a living, breathing entity that constantly interacts with its environment, including the food you eat, the medications you take, and the stress you experience. Think of it as a bustling metropolis, with various neighborhoods (different species of bacteria) working together to keep the city (your body) running smoothly. When everything is in balance, your gut microbiome supports digestion, synthesizes essential vitamins, helps regulate your immune system, and even communicates with your brain via the gut-brain axis.
But this balance is delicate. Disruptions can occur easily, leading to a state known as dysbiosis—a microbial imbalance that can trigger a cascade of health problems. This imbalance can be caused by a variety of factors, including diet, stress, and yes, medications, particularly those we often reach for without a second thought.
The Delicate Balance of Gut Flora
The balance of gut flora is not just a matter of having the right number of bacteria. It’s about diversity, stability, and the right mix of species that work in harmony. When this balance is disrupted, it’s like throwing a wrench into a finely tuned machine.
Dysbiosis, or an imbalance in the gut microbiome, has been linked to a range of health issues, from gastrointestinal disorders like irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) to systemic conditions like obesity, diabetes, and even mental health disorders like anxiety and depression. The gut microbiome’s influence is so profound that some scientists refer to it as our “second brain,” underscoring its role in overall health.
So, what happens when something disrupts this balance? Let’s say you’ve taken an antibiotic to clear up a bacterial infection. While the antibiotic does its job by killing the harmful bacteria, it doesn’t discriminate—it also wipes out beneficial bacteria in your gut, creating an opportunity for harmful bacteria to overgrow. Similarly, the repeated use of certain OTC medications can lead to long-term changes in gut flora, potentially setting the stage for dysbiosis.
With this understanding of the gut microbiome in mind, let’s explore how OTC medications can affect this delicate ecosystem, sometimes with unintended consequences.
When you sit on the toilet, your hips are in a flexed position, which can make it harder for your colon to do its job. Using The PoopSTICK can help alleviate this issue, making it easier to pass poop and reduce the discomfort associated with constipation.

NSAIDs and Gut Health
Non-steroidal anti-inflammatory drugs (NSAIDs) are some of the most commonly used OTC medications. They’re the go-to for everything from headaches and menstrual cramps to arthritis and muscle pain. But while they’re effective at quelling pain and inflammation, they come with a hidden cost—particularly when it comes to gut health.
NSAIDs work by blocking the enzymes COX-1 and COX-2, which are involved in the production of prostaglandins. Prostaglandins are compounds that promote inflammation, pain, and fever, so inhibiting their production can provide relief from these symptoms. However, prostaglandins also play a crucial role in protecting the lining of your stomach and intestines.
When you take NSAIDs, you’re not just reducing pain—you’re also reducing the production of protective prostaglandins. This can lead to a thinning of the protective mucous layer in your stomach and intestines, making them more susceptible to damage from stomach acid. Over time, this can result in gastritis (inflammation of the stomach lining), ulcers, and even gastrointestinal bleeding. These effects can be particularly pronounced with long-term or frequent use of NSAIDs.
Moreover, NSAIDs have been shown to disrupt the balance of gut bacteria. Studies have found that NSAID use can decrease the diversity of the gut microbiome, reducing the abundance of beneficial bacteria while allowing harmful bacteria to proliferate. This shift in gut flora can lead to dysbiosis, increasing the risk of conditions like irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD).
In short, while NSAIDs are effective for pain relief, they should be used with caution, especially if you’re concerned about your gut health. Overuse or chronic use can lead to serious gastrointestinal issues that could outweigh the benefits of the medication.
Antacids and Acid Suppressants
Heartburn, acid reflux, and indigestion are common ailments that many of us experience from time to time. When that familiar burning sensation strikes, it’s easy to reach for an antacid or acid suppressant to neutralize the acid and provide quick relief. However, these medications, while effective in the short term, can have unintended consequences on your gut health when used frequently or over long periods.
Antacids work by neutralizing stomach acid, while acid suppressants like proton pump inhibitors (PPIs) reduce the production of stomach acid. Stomach acid is crucial for breaking down food, absorbing nutrients, and killing harmful bacteria that enter the stomach. When you reduce stomach acid too much, it can interfere with these processes.
One of the main concerns with long-term use of antacids and acid suppressants is that they can alter the environment of the gut, leading to an overgrowth of harmful bacteria. For example, low stomach acid can create an environment where bacteria that normally wouldn’t survive in the acidic conditions of the stomach can thrive. This can lead to small intestinal bacterial overgrowth (SIBO), a condition where too many bacteria grow in the small intestine, causing symptoms like bloating, gas, diarrhea, and malabsorption of nutrients.
In addition to SIBO, long-term use of acid suppressants has been linked to an increased risk of Clostridioides difficile (C. diff) infection, a serious bacterial infection that can cause severe diarrhea and colitis. The reduction in stomach acid can also impair the absorption of essential nutrients like calcium, magnesium, and vitamin B12, potentially leading to deficiencies over time.
While antacids and acid suppressants can provide much-needed relief from occasional heartburn or acid reflux, it’s important to use them judiciously and to explore other ways to manage symptoms, such as dietary changes or lifestyle modifications.
Laxatives and Gut Motility
Constipation is another common issue that many people face, and when it strikes, reaching for a laxative can seem like a quick and easy solution. Laxatives work by either drawing water into the bowel to soften stool, stimulating bowel movements, or adding bulk to stool to help it pass more easily. While laxatives can be effective for relieving constipation, their overuse can lead to problems that go beyond just dependency.
One of the main concerns with the overuse of laxatives is that they can interfere with the natural motility of the gut. The gut has its own rhythmic contractions, known as peristalsis, which move food and waste through the digestive tract. When you rely on laxatives to stimulate these contractions, your gut may become “lazy,” leading to a condition known as laxative dependence. This means that your gut may not function properly without the aid of laxatives, making it difficult to have a bowel movement on your own.
In addition to affecting gut motility, laxatives can also disrupt the balance of gut bacteria. For example, osmotic laxatives, which work by drawing water into the bowel, can alter the gut’s environment, potentially leading to shifts in the gut microbiome. Similarly, stimulant laxatives, which trigger contractions in the gut, can also affect the composition of gut bacteria, particularly if used frequently or over long periods.
Furthermore, some laxatives, particularly stimulant laxatives, can cause inflammation of the gut lining if used excessively. This can lead to a condition known as cathartic colon, where the colon becomes distended and less effective at moving stool through the digestive tract. Over time, this can lead to chronic constipation, dependence on laxatives, and potentially more serious gastrointestinal issues.
If you’re struggling with constipation, it’s important to explore other options for managing it, such as increasing fiber intake, staying hydrated, and getting regular exercise. While laxatives can provide relief, they should be used sparingly and under the guidance of a healthcare professional.
Cold Medications and Gut Health
Cold and allergy medications are staples in most medicine cabinets, especially during the fall and winter months when colds and flu are most common. These medications can help relieve symptoms like congestion, runny nose, and cough, allowing you to get through your day with a little more ease. However, like other OTC medications, cold medications can also affect your gut health, particularly if used frequently.
Many cold medications contain decongestants, antihistamines, or a combination of both. Decongestants like pseudoephedrine work by constricting blood vessels in the nasal passages, reducing swelling and congestion. While effective, decongestants can also cause side effects like dry mouth, constipation, and in some cases, gastrointestinal discomfort. Antihistamines like diphenhydramine, which block histamine receptors to reduce allergy symptoms, can also cause constipation by slowing down gut motility.
In addition to these side effects, some cold medications contain ingredients that can disrupt the gut microbiome. For example, certain cough syrups and lozenges contain high amounts of sugar or artificial sweeteners, which can feed harmful bacteria in the gut and contribute to dysbiosis. While these effects may be mild and temporary with occasional use, frequent use of cold medications, especially those with added sugars or artificial ingredients, can have a more lasting impact on gut health.
If you find yourself reaching for cold medications frequently, it may be worth exploring other ways to manage symptoms, such as using a humidifier, staying hydrated, and getting plenty of rest. Natural remedies like honey, ginger, and herbal teas can also help soothe symptoms without the potential side effects of OTC medications.

Chronic Gastrointestinal Issues
The gut is often considered the gateway to overall health, and when it’s compromised, the consequences can be far-reaching. Chronic use of OTC medications can disrupt the delicate balance of the gut microbiome, leading to long-term gastrointestinal issues that can significantly impact your quality of life.
One of the most common conditions associated with disrupted gut health is irritable bowel syndrome (IBS). IBS is a chronic disorder that affects the large intestine, causing symptoms like abdominal pain, bloating, gas, diarrhea, and constipation. While the exact cause of IBS is unknown, research suggests that changes in the gut microbiome, particularly an overgrowth of harmful bacteria, may play a role in triggering and exacerbating symptoms. Frequent use of NSAIDs, laxatives, or antacids can contribute to these microbial changes, potentially increasing the risk of developing IBS.
Another condition linked to disrupted gut health is gastroesophageal reflux disease (GERD). GERD occurs when stomach acid frequently flows back into the esophagus, causing symptoms like heartburn, chest pain, and difficulty swallowing. While GERD is often treated with acid suppressants, these medications can also contribute to dysbiosis, potentially worsening symptoms over time. Moreover, long-term use of acid suppressants has been associated with an increased risk of developing conditions like Barrett’s esophagus, a precursor to esophageal cancer.
Small intestinal bacterial overgrowth (SIBO) is another condition that can arise from dysbiosis. SIBO occurs when there is an abnormal increase in the number of bacteria in the small intestine, leading to symptoms like bloating, gas, diarrhea, and malabsorption of nutrients. SIBO can be triggered by a variety of factors, including the use of antibiotics, acid suppressants, and certain laxatives. If left untreated, SIBO can lead to nutrient deficiencies, weight loss, and chronic digestive issues.
These are just a few examples of how chronic disruption of the gut microbiome can lead to long-term gastrointestinal issues. The key takeaway is that while OTC medications can provide relief from symptoms, they should be used with caution, particularly if you have a history of gut-related issues.
Immune System Impact
The gut is home to a significant portion of the body’s immune system, with up to 70% of immune cells residing in the gut. This makes the gut microbiome a crucial player in immune function, helping to protect against pathogens, regulate inflammation, and maintain overall immune balance.
When the gut microbiome is disrupted by factors like frequent use of OTC medications, it can have a ripple effect on the immune system. Dysbiosis can lead to an overactive immune response, resulting in chronic inflammation, which has been linked to a wide range of health issues, including autoimmune diseases, allergies, and chronic inflammatory conditions like rheumatoid arthritis and inflammatory bowel disease.
Moreover, a compromised gut microbiome can make the body more susceptible to infections. For example, low stomach acid caused by frequent use of acid suppressants can reduce the body’s ability to kill harmful bacteria that enter the stomach, increasing the risk of infections like C. diff and Helicobacter pylori. Similarly, disruptions in gut flora caused by antibiotics or NSAIDs can reduce the abundance of beneficial bacteria that help protect against pathogenic invaders.
On the flip side, a healthy gut microbiome supports a robust immune system by producing short-chain fatty acids (SCFAs) like butyrate, which have anti-inflammatory properties and help maintain the integrity of the gut lining. Beneficial bacteria in the gut also play a role in training the immune system to distinguish between harmful pathogens and harmless antigens, reducing the risk of immune-related disorders.
Given the strong connection between the gut and the immune system, it’s important to be mindful of how OTC medications might be affecting this delicate balance. Supporting gut health through diet, probiotics, and lifestyle changes can help maintain a healthy immune system and reduce the risk of chronic inflammation and infections.
Mental Health Connections
The gut and the brain are inextricably linked through a complex network of nerves, hormones, and biochemical signaling molecules—a relationship often referred to as the gut-brain axis. This connection means that changes in gut health can have a direct impact on mental health, influencing everything from mood and anxiety to cognitive function and stress response.
One of the most well-studied aspects of the gut-brain axis is the role of gut bacteria in the production of neurotransmitters like serotonin, dopamine, and gamma-aminobutyric acid (GABA). Serotonin, in particular, is of interest because approximately 90% of the body’s serotonin is produced in the gut. This neurotransmitter plays a key role in regulating mood, sleep, and appetite, and imbalances in serotonin levels have been linked to conditions like depression and anxiety.
When the gut microbiome is disrupted by factors like chronic use of OTC medications, it can lead to changes in the production and regulation of these neurotransmitters. For example, dysbiosis has been associated with reduced levels of beneficial bacteria that produce SCFAs, which are important for maintaining the blood-brain barrier and modulating inflammation in the brain. This can contribute to symptoms of anxiety, depression, and cognitive decline.
Moreover, chronic inflammation in the gut, which can be triggered by the overuse of NSAIDs or acid suppressants, has been linked to increased levels of inflammatory cytokines in the brain. These cytokines can interfere with neurotransmitter signaling and have been implicated in the development of mood disorders like depression and anxiety.
There’s also emerging evidence that the gut microbiome plays a role in the body’s stress response. Dysbiosis can lead to an overactive hypothalamic-pituitary-adrenal (HPA) axis, which regulates the body’s response to stress. This can result in heightened levels of cortisol, the stress hormone, which has been linked to a range of mental health issues, including anxiety, depression, and sleep disorders.
Given the strong connection between gut health and mental health, it’s important to consider how OTC medications might be affecting this relationship. Supporting a healthy gut through diet, probiotics, and stress management techniques can help maintain balance in the gut-brain axis, promoting better mental health and overall well-being.

Consult a Healthcare Professional
Before reaching for an OTC medication, it’s always a good idea to consult with a healthcare professional, especially if you plan to use the medication frequently or over a long period. A doctor or pharmacist can help you understand the potential risks and benefits of the medication, recommend alternatives, and guide you on how to use it safely.
If you have a history of gastrointestinal issues, such as IBS, GERD, or dysbiosis, it’s particularly important to discuss your options with a healthcare provider. They can help you identify the root cause of your symptoms and suggest treatments that are less likely to disrupt your gut health.
Use OTC Medications Sparingly
OTC medications are best used as a short-term solution for occasional symptoms. Whenever possible, try to limit your use of these medications and opt for natural remedies or lifestyle changes instead. For example, instead of relying on NSAIDs for chronic pain, consider incorporating anti-inflammatory foods into your diet, practicing yoga or meditation for stress relief, and exploring physical therapy or acupuncture for pain management.
Similarly, if you frequently experience heartburn or acid reflux, consider making dietary changes, such as avoiding trigger foods, eating smaller meals, and not lying down immediately after eating, rather than relying on antacids or acid suppressants.
Incorporate Gut-Friendly Practices
Supporting your gut health through diet and lifestyle can help protect against the potential negative effects of OTC medications. Here are some gut-friendly practices to consider:
Probiotics and Prebiotics: Probiotics are beneficial bacteria that can help restore balance to the gut microbiome, while prebiotics are fibers that feed these bacteria. Incorporating probiotic-rich foods like yogurt, kefir, sauerkraut, and kimchi into your diet, along with prebiotic-rich foods like garlic, onions, and bananas, can help support a healthy gut.
Fiber-Rich Diet: A diet high in fiber can promote regular bowel movements and support a healthy gut microbiome. Aim to include a variety of fruits, vegetables, whole grains, and legumes in your diet.
Stay Hydrated: Drinking plenty of water is essential for maintaining healthy digestion and preventing constipation. Aim to drink at least 8 glasses of water a day, and more if you’re physically active or live in a hot climate.
Regular Exercise: Physical activity can help stimulate gut motility and promote regular bowel movements. Aim for at least 30 minutes of moderate exercise most days of the week.
Stress Management: Chronic stress can negatively impact gut health by disrupting the gut-brain axis and contributing to dysbiosis. Incorporating stress management techniques like mindfulness meditation, deep breathing exercises, and regular physical activity can help support a healthy gut.
Natural Alternatives
If you’re looking for alternatives to OTC medications, there are plenty of natural remedies that can help manage symptoms without the potential side effects. Here are a few to consider:
Ginger: Ginger is a natural anti-inflammatory that can help relieve nausea, indigestion, and pain. Try drinking ginger tea or adding fresh ginger to your meals.
Turmeric: Turmeric contains curcumin, a compound with powerful anti-inflammatory properties. Incorporating turmeric into your diet, either as a spice or in supplement form, can help reduce inflammation and pain.
Peppermint: Peppermint oil has been shown to relax the muscles of the gastrointestinal tract, making it an effective remedy for symptoms of IBS and indigestion. Try drinking peppermint tea or using peppermint oil capsules.
Aloe Vera: Aloe vera is known for its soothing properties and can help relieve symptoms of acid reflux and indigestion. Look for aloe vera juice that is specifically formulated for internal use.
Magnesium: Magnesium is a natural muscle relaxant that can help relieve constipation. You can increase your magnesium intake through foods like leafy greens, nuts, and seeds, or by taking a magnesium supplement.
The PoopSTICK: Sometimes, natural relief from constipation can be as simple as changing your posture. The PoopSTICK is a simple device designed to elevate your feet while sitting on the toilet, mimicking a squatting position. This position straightens the colon, making it easier and more natural to eliminate waste. Unlike traditional laxatives, The PoopSTICK offers a non-invasive, drug-free method to help promote regular bowel movements, reduce straining, and support overall gut health.
.

As we’ve explored, while over-the-counter medications can offer quick relief from a variety of ailments, they are not without their potential downsides, particularly when it comes to gut health. The gut microbiome is a delicate and complex system that plays a crucial role in our overall health, from digestion and immunity to mental well-being. Disrupting this balance through the overuse or misuse of OTC medications can lead to a host of gastrointestinal issues, weakened immune function, and even mental health challenges.
The good news is that by being mindful of how we use these medications and taking steps to support our gut health, we can mitigate these risks. Whether it’s consulting with a healthcare professional, using medications sparingly, incorporating gut-friendly practices, or exploring natural alternatives like The PoopSTICK, there are plenty of ways to protect your gut while still managing your symptoms effectively.
So next time you reach for that bottle of pain relievers or antacids, take a moment to consider your gut health. By making informed choices and adopting a holistic approach to wellness, you can ensure that you’re not just treating your symptoms, but also supporting your long-term health and well-being.

Your scale isn’t measuring fat — it’s measuring what your gut hasn’t let go of. Hidden stool retention, slow motility, and gut bacteria can quietly

Your poop is a real-time report card on your gut health—and most people are ignoring it. From color changes to weird shapes to the clues

Wheat isn’t the villain—it’s the kind of wheat that’s wrecking your gut. From ancient grains to modern hybrids, discover how today’s wheat triggers inflammation, worsens

Your gut isn’t just digesting food—it’s controlling your hunger, energy, and even how fast you burn fat. Inside you is a powerful hormone called GLP-1,

Happy Poops.
What about your friends?